There are several different categories of glaucoma which include: Open Angle Glaucoma, Narrow Angle Glaucoma, Congenital Glaucoma and Secondary Glaucoma.

Different Types of Glaucoma
Open Angle Glaucoma
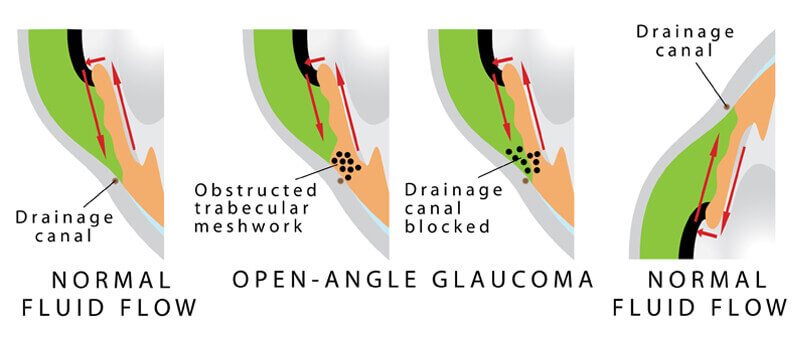
Open Angle Glaucoma is the most common form of glaucoma and is a result of the trabecular meshwork becoming less efficient over time. In this case, the eye continues to produce the same amount of aqueous humor, but the trabecular meshwork is not able to keep up. This imbalance of fluid production and drainage results in an excess amount of aqueous fluid. As the fluid builds up, the intraocular pressure (IOP) elevates. As a consequence to this elevation in eye pressure, the optic nerve becomes damaged.
Glaucome vision lossFor most people with open angle glaucoma, there are no perceivable symptoms in the early stages of the disease. However, as the optic nerve is continually subjected to an environment of increased eye pressure, it becomes damaged. This damage is eventually perceived as peripheral visual field defects. If the eye pressure is not monitored or controlled, open angle glaucoma can eventually lead to blindness.
An ideal intraocular pressure is different for each individual. Some patients are able to tolerate a higher eye pressure while others cannot. It is important to be followed regularly by your eye doctor to determine an appropriate target IOP and ensure that this pressure is maintained over time.
Narrow Angle Glaucoma
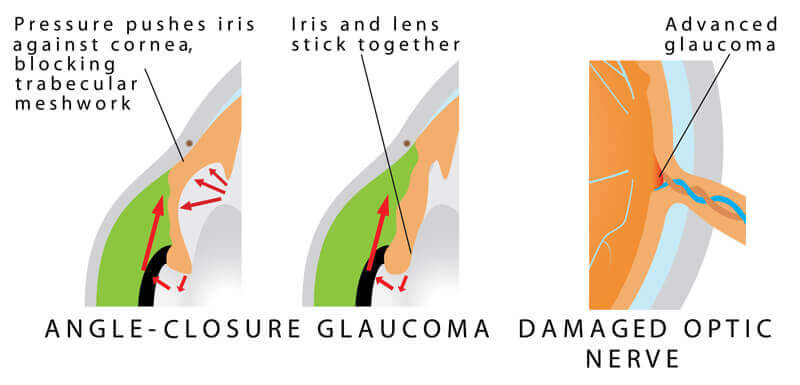
Narrow Angle Glaucoma is less common than Open Angle Glaucoma. People who are farsighted (hyperopic) are more susceptible to this form of glaucoma because they typically have smaller eyes, although Narrow Angle Glaucoma can occur in nearsighted eyes. A smaller eye correlates to more crowding of the structures within the eye. In a normal eye there is sufficient space between the iris (the colored part of the eye) and the trabecular meshwork. However, in a crowded eye, the space between the iris and the trabecular meshwork is narrowed.
The iris controls the amount of light that enters the eye. Under bright light conditions the iris contracts to cover more space and make the pupil smaller (minimizing the amount of light that enters the eye). In dark lighting conditions, the iris dilates to allow more light to enter the eye. In a person with narrow angles, as the pupil dilates the iris can completely block the trabecular meshwork drainage angle. This can result in a rapid rise in eye pressure and can lead to an angle closure glaucoma attack.
An individual suffering from an angle closure attack typically experiences a severe headache above the eye brow, eye pain, significant eye redness, the pupil becomes fixed and dilated, the vision is significantly blurred, halos are seen around lights and nausea and vomiting can occur. An angle closure glaucoma attack is an emergency and must be treated immediately. Unfortunately, the damage done to the optic nerve during an angle closure glaucoma attack can be significant and is permanent. In some cases, Angle Closure Glaucoma can present insidiously however, without sudden symptoms.
Preventing Angle Closure
Fortunately, there is a means of preventing angle closure attacks. Narrow angles can be diagnosed during a routine eye exam. At that time, the doctor will look at the trabecular meshwork drainage angle through a special contact lens. This testing, referred to as gonioscopy, allows the doctor to determine the degree of narrowing. If the angles are very narrow, the doctor may recommend a laser procedure known as Laser Peripheral Iridotomy. During this in-office (out-patient) procedure, a small hole is created in the iris. This microscopic hole allows for another route for the aqueous fluid to enter the anterior chamber, and allows the iris to fall away from the drainage angle. The doctor makes the hole on the top part of the iris that is usually covered by the eyelid.
As with any surgical procedure, there are some risks to Laser Peripheral Iridotomy. However, the risks of the procedure are minimal and if the procedure is recommended, the benefit of the procedure in reducing the risk of angle closure glaucoma outweighs the risk of the procedure. Some of the risks include blurred vision, slight bleeding or inflammation within the eye. Some people notice a twinkle or flicker of light or shadow image after the procedure. These symptoms can arise from the affect of light entering the small hole in the iris. This side effect of the procedure is very unusual; in most cases, the upper eyelid covers the location of the iridotomy and the optical side effect is not perceived. Occasionally, the procedure needs to be repeated if the iridotomy heals over.
Congenital Glaucoma
Congenital Glaucoma is a result of the malformation of the trabecular meshwork drainage angle during fetal development. The defective trabecular meshwork impedes the proper drainage of the aqueous fluid within the eye causing an increase in intraocular pressure. The elevated eye pressure eventually leads to damage of the optic nerve, which may result in blindness. For this reason it is imperative that children afflicted by the disease be seen by an ophthalmologist regularly in hopes of preserving as much of the child’s vision as possible.
Congenital glaucoma is generally diagnosed within the first few months of a child’s life. Infants with congenital glaucoma often have symptoms of tearing, red eye, light sensitivity and a cloudy appearance of the eye. In the far majority of congenital glaucoma cases, both eyes are affected by the disease. Males are more commonly afflicted with this disease than females; however, congenital glaucoma is rare, affecting approximately 0.05% of children.
Secondary Glaucoma
Secondary glaucoma is an acquired form of glaucoma and may present itself as open angle or angle closure glaucoma. This type of glaucoma can be a result of trauma, inflammatory diseases, tumors or use of corticosteroids. Secondary glaucoma may be temporary.
Traumatic Secondary Glaucoma
In the circumstance of either blunt or penetrating ocular trauma, the trabecular meshwork can be damaged. This damage leads to the trabecular meshwork inefficiently draining the aqueous fluid out of the eye. As a result, the amount of aqueous fluid in the eye builds and increases the intraocular pressure. This increase in eye pressure leads to damage of the optic nerve. Eventually, the optic nerve damage results in visual field defects, and in some cases blindness.
Inflammatory Glaucoma and Steroid Responders
Inflammatory diseases such as uveitis can also lead to secondary glaucoma. Additionally, most cases of uveitis are treated with corticosteroids. Unfortunately, one of the side effects of corticosteroid use can be a significant increase in intraocular pressure. This cyclic condition is often a tight-rope-walk for the ophthalmologist to effectively treat the ocular inflammation while trying to maintain an adequate intraocular pressure.
Pseudoexfoliative Glaucoma
One of the more common forms of secondary glaucoma is referred to as pseudoexfoliation glaucoma. This type of secondary glaucoma occurs when the eye forms material that can affect the drainage angle. Like a clogged sink, the fluid is unable to properly drain and fluid accumulates within the eye. This accumulation of fluid can lead to an increase in eye pressure and eventually damage the optic nerve.
Pigmentary Glaucoma
Similarly, pigmentary glaucoma is another form of secondary glaucoma. Pigmentary glaucoma is a result of the iris pigment breaking off. These pigment granules can then clog the drainage angle and induce glaucoma.
Neovascular Glaucoma
Neovascular glaucoma is another form of secondary glaucoma. This form of glaucoma typically affects individuals with diabetes, or eyes that have circulation problems in the retina or in the arteries that supply the eye. Neovascularization refers to the new growth of abnormal blood vessels. The new blood vessels can block the trabecular meshwork and lead to high eye pressure. This form of glaucoma can be difficult to treat.
ICE Syndrome
ICE is an acronym for, “IridoCorneal Endothelial” syndrome. This is a very rare form of glaucoma that typically affects one eye. The condition occurs when the endothelial layer (the most inner layer) of the cornea grows over the trabecular meshwork and across the surface of the iris. This causes an increase in intraocular pressure and leads to damage of the optic nerve. These abnormal endothelial cells form adhesions that attach the iris to the cornea, which in turn blocks the drainage angle further.


