Cataracts develop as part of the natural aging process within the eye. Currently, there are no medications, eye drops or exercises that can prevent a cataract from forming. Cataract surgery is the only way to remove a cataract that is causing visual problems. When cataracts become visually significant and begin to interfere with your normal daily tasks, cataract surgery may be considered.
Prior to surgery, a series of eye drops are instilled to dilate the pupil. A local anesthetic is used to numb the eye. Also, a mild sedative is administered intravenously to make the patient more relaxed and comfortable during surgery.
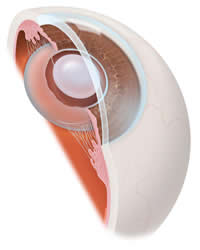
IOL in placeDuring cataract surgery, a small incision is made near the outer edge of the cornea. A small instrument is used to remove the front portion of the capsule to access the cataract. An ultrasonic probe is used to break up the cataract using ultrasonic waves. This technique is referred to as phacoemulsification. Once the cataract is broken up into tiny lens fragments, these fragments are suctioned out of the capsule and removed from the eye. In most cases, an intraocular lens is then oriented into the empty lens capsule. This lens has special arms that hold it in place.
In most cases, the surgical wound is so small that it does not require the use of stitches, but sutures are placed if needed for safety. After surgery, a patch is placed over the operative eye. The patch will remain in place until it is removed in the office the day after surgery. At that time, a postoperative eye drop regimen will be initiated.
Risks of Cataract Surgery
Although cataract surgery is considered one of the safest and most effective surgical procedures performed in the United States, there are still risks involved. For this reason, cataract surgery should not be considered lightly. It is up to the patient and surgeon to determine when cataract surgery is appropriate. For most people this is when the level of vision is interfering with day-to-day activities and the benefits of surgery outweigh the risks.
In order for a patient to decide whether or not to proceed with cataract surgery, it is important to understand the risks and benefits of surgery. Fortunately, cataract surgery has a very high success rate with the vast majority of patients experiencing no complications at all. That being said, there are risks associated with any surgical procedure. In rare cases, there can be the need for additional surgery or permanent loss of vision as a result of complications due to cataract surgery. Below you will find a list of risks of cataract surgery that happen rarely, but can occur, and include but are not limited to:
- Damage to a structure in or around the eye that may lead to additional surgery
- Bleeding that can cause loss of vision (this may be temporary or permanent)
- Detachment of the retina or a retinal tear
- Infection that may require additional medicines and treatments
- Swelling of the front of the eye (corneal edema) that can result in discomfort, decreased vision and may necessitate additional surgery, medicines (such as eye drops or ointments) or treatments
- Macular edema (swelling of the macula) that may require additional medicines (such as eye drops) or treatments
- Chronic eye inflammation (iritis/uveitis) that may necessitate additional treatments or medications
- Increased intraocular pressure that may lead to glaucoma and the need for eye drops, additional treatments, and in rare cases, surgery
- Diplopia (double vision), treatable with special glasses lenses in most cases
- Anisometropia (asymmetrical vision) or astigmatism
- Dislocation of the natural crystalline lens or dislocation of the intraocular lens which may result in additional surgery
- Ptosis (droopy eyelid) that may be only temporary after surgery, or can be constant; chronic ptosis can be surgically repaired
- Anisocoria (difference in pupil size) or misshapen pupils
- Unsatisfactory outcome due to a preexisting ocular condition (such as macular degeneration or amblyopia)
- Vision loss, blindness or loss of the eye


