Glaucoma Testing

There are several tests that help doctors to detect and monitor glaucoma. The first tests include measuring the intraocular pressure with tonometry and observing the optic disc. Other testing may include, but is not limited to, visual fields, pachymetry, gonioscopy, dilated exams, photography of the optic disc and optical coherence tomography (OCT).
Tonometry
The intraocular pressure is measured through a technique called, tonometry. This measurement is quantified in millimeters of mercury (mm Hg); “normal” eye pressure is considered to be within the range of 10-21 mm of Hg. That being said, an ideal intraocular pressure is different for each individual. Some patients are able to tolerate a higher eye pressure while others cannot. Your eye doctor will be able to determine what target eye pressure is appropriate for you.
Visual Field Testing

The Humphrey Visual Field is able to assess the peripheral vision. During this test a patient is asked to fixate on a central light target. Throughout the test, lights appear to the side of the vision (differing in size and brightness). The patient is instructed to compress a controller each time s/he perceives a light. The test is able to map the visual field and illustrates any visual areas that have been lost due to glaucomatous damage. Each eye is tested individually because glaucoma may affect the eyes asymmetrically.
In a normal eye there is only one blind spot. This blind spot occurs at the area where the optic nerve and blood vessels enter the retina (therefore, no visual signal can be sent to the brain in this area). However, if damage is done to the optic nerve due to glaucoma, additional areas of blind spots will appear on the visual field test.
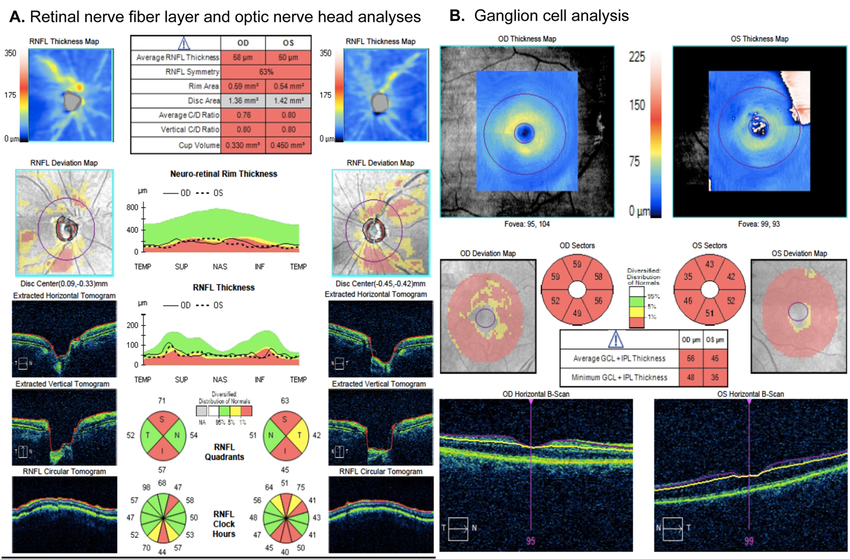
OCT
OCT is an acronym for “Optical Coherence Tomography”. This state-of-the-art instrument is used to analyze the anatomic structure of the optic nerve head, or disc, and the retina. This instrument and the tests it can perform are very useful for the evaluation of the optic nerve and macula to diagnose conditions such as thinning of the optic nerve, macular holes, epi-retinal membranes, cystoid macular edema, central serous choroidopathy and diabetic retinopathy.
The test itself is quick and painless and involves a noninvasive/noncontact scan of the internal structures of the eye. The data is generated via optical backscattering of light and produces cross sectional images of the retina and the optic nerve head. This sophisticated technology boasts extremely high micrometer-resolution that generates a three dimensional image. As a result, OCT testing allows for the layers of the retina to be isolated and differentiated, thus determining the thickness of the retina.
OCTs are able to provide a snap-shot in time. Comparison of past and present OCTs allows for monitoring of small changes over time. For this reason, OCT testing has proved to be a vital tool when evaluating such conditions as glaucoma and macular changes.
Central Corneal Thickness
The central corneal thickness is measured with an instrument called a pachymeter. During this test, safe ultrasonic sound waves are used to determine the corneal thickness (in units of microns). This is an important measurement because tonometry is based upon a “normal” corneal thickness. However, if an individual has a thicker or thinner corneal thickness, the eye pressure can be adjusted to compensate for this difference. For instance, if the corneal tissue is thicker than average, the tonometry reading is artificially high; whereas if the cornea is thinner than average, the tonometry reading is artificially low.
Gonioscopy
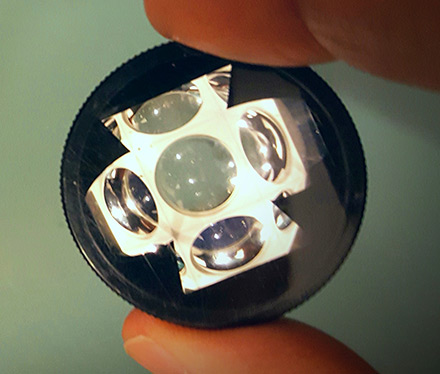
This is a painless test that allows the doctor to view the drainage angle in the eye. During a gonioscopy exam, the doctor holds a small contact lens over the eye, after the eye is anesthetized with an eye drop. The view allows the doctor to grade the angle of the eye (the space between the cornea and the iris). This determination can verify whether a patient has an open angle, narrow angle or closed angle.
Dilated Eye Exam
Dilated eye exams allow the doctor to view the retina through a series of special lights and lenses. During this exam, the doctor is able to assess the appearance of the optic nerve. Typically, the optic nerve is graded based upon a cup-to-disc ratio (a scale between 0.0 and 1.0). A normal optic disc has a certain amount of typical cupping; however, glaucoma can induce additional pathological cupping of the optic disc. The outer rim of the optic nerve contains nerve fibers that, in a healthy eye, appear sharp and pink. The inner white cup is referred to as the “pit” and has no nerve fibers. In a person with glaucoma, the cup enlarges over time until it occupies the majority of the disc area.
The cup-to-disc ratio is based upon a relationship of the diameter of the “cup” portion of the disc in comparison with the total diameter of the optic disc. A better way to visualize the cup-to-disc ratio is to consider the hole in a bagel or donut; the hole represents the cup and the surrounding dough is the disc. If the cup fills one tenth (1/10) of the disc, the resulting ratio is 0.1; on the contrary, if the cup comprises 8/10 of the disc, the ratio is 0.8. The larger the cup-to-disc ratio, the more suspicious the eye is for glaucoma. Glaucoma cannot be diagnosed solely on the appearance of the optic nerve cup-to-disc ratio, but it is an important indicator. For instance, if the cup-to-disc ratio continues to increase over time, the patient may be diagnosed with glaucoma. Although some individuals are simply born with a higher than average cup-to-disc ratio that may remain stable throughout his/her lifetime.


